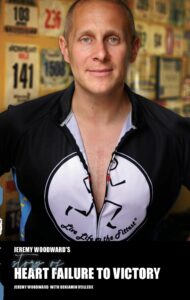
The following excerpt is from “Jeremy Woodward’s Story of Heart Failure to Victory,” a book recently released by the Concord native and fitness trainer. This chapter picks up in 2007 at Tufts Medical Center in Boston as Jeremy, then 25, prepares for open-heart surgery. It was there that he made a commitment that would come to shape his recovery and redefine his purpose.
“Jeremy, I don’t think you’re fully processing this right now, so let me put it bluntly. If you leave this hospital, I strongly believe that you will not make it back in alive.”
After hearing those fateful words, I thought I’d be rushed into surgery. I was completely wrong. The doctors moved quickly to get me situated, but it was in a hospital room, not an operating room. While I was happy to be receiving treatment, I felt a slight sense of disdain at seeing the inside of a hospital room again. I was hoping that I wouldn’t have to stay there for observation for a week, like I had for my initial tissue valve surgery. Well, my hopes came true: I didn’t end up staying a week.
I ended up staying for much longer.
The doctors predicted that the surgery preparations would take two to four weeks. I was not happy about this at all, but I didn’t have much time to dwell on it. I hadn’t been in my room for five minutes before I received a dose of sedatives. I had just enough time to think, ‘Man, I hope these drugs kick in soon’ before I blacked out.
I woke up in a fog. It took a few seconds to remember where I was. I struggled to sit up. The first thing I noticed was that I had dozens of wires, patches and tubes hooked up to me. I looked like the inside of a computer. Looking to either side of my bed showed that there were many more machines surrounding me than I expected. Some beeped in time with my heart, others occasionally flickered with lights, and others just sat there serving an unknown purpose.
Even though I had slept for a long time (it looked to be morning outside) I felt as if I had only taken a cat nap. I was sore. I didn’t feel any better than when I had been admitted, but I also didn’t feel any worse. I took that as a good sign. I shifted myself back down in the bed and closed my eyes.
I slept almost the entire second day away. I woke up to a nurse taking readings and measurements from the machines. I mumbled a greeting to her, and she smiled in return.
“Good afternoon! How are you feeling?” I sat up in bed, and to my surprise, I felt a lot less sore.
“Wow, I’m already feeling better!” I exclaimed. I felt around my legs and stomach and noticed that there was a notable decline in fluid. It wasn’t a drastic change, but it was certainly a great start. A smile formed on my face for the first time in a long while. I turned and saw Brook sitting next to me, beaming in joy at the quick turnaround.
“Are you hungry?” the nurse asked. Again, to my pleasant surprise, I had a decent appetite.
“Yeah, I’d say so. Is it dinner time?”
“It’s your call, late lunch or early dinner. Here, look at our menu and see what you think,” the nurse suggested as she handed me a laminated sheet of paper. One side listed the breakfast and lunch options while the other side displayed the dinner and snack choices. I scanned through the lunch options and liked what I saw, but nothing stuck out as a good option at the time. I flipped the menu over and browsed the selection of dinner choices. My gaze settled on ‘hospital chicken stir fry’. Reading the description made me salivate. I gave the rest of the items a once-over, but none sounded as good as the stir fry.
“Could I have the hospital chicken stir fry, please?”
“Absolutely. In the meantime, if you could take these along with some water, that would be great.” She handed me a paper cup with several pills in it and a matching cup filled with water. I took both, tossing the pills back and chasing them with the water as the nurse walked out of the room, menu in hand. As she left, I turned to look at Brook. She smiled and took my hand.
“So you’re feeling better?” she asked tentatively, squeezing my hand. I nodded my head in response, describing how I could feel that the fluid had already gone down a little bit. “The doctors have discussed surgery options with me, and I think that a mechanical valve implant is the smart decision,” said my wife. She went on to explain the process, benefits and specifics involved. A mechanical valve would function more efficiently than a tissue valve would. Also, a mechanical valve would last almost three times as long as a tissue valve before requiring surgical maintenance. To further cement the decision, I wasn’t keen on undergoing another tissue valve replacement with the experience I had just gone through, and an entire heart transplant seemed so cumbersome and intensive. After discussing logistics and other details, I agreed with Brook on a valve replacement. A mechanical valve would need more minute upkeep in the form of daily Coumadin intake to keep the valve clean, but the thirty-year comparison versus a tissue valve’s life expectancy of ten to fifteen was what really helped make the decision for me.
Just as we finished discussing the surgery, the nurse returned to the room with a plate piled high with steaming food. My eyes fixated on the food that was fast approaching. It turned out that I was hungrier than I thought. The first bite of the stir fry tasted amazing. I almost let out a cry of joy at how good it was. After cleaning the plate Brook and I talked for another hour. She then kissed me goodbye and left for home, as she had to work the next morning.
Over the next week, I ordered the same meal for dinner every night. After several days, the nurse didn’t even bother to bring in the menu for dinner. My only complaint in terms of food and drink was that I was very limited with my liquid intake. I was only allowed to have a small amount of liquid per day due to the built-up fluid in my legs and stomach. In addition, I was on a high dose of diuretics for the first ten days. Due to these diuretics, I was going to the bathroom an insane amount. I felt like my body was going to dry out like a sponge. Luckily, the only things that dried out were the concentrations of fluid in my legs and stomachs. Every day they looked and felt smaller than the previous day.
Unfortunately, I couldn’t just get up out of my bed and go to the bathroom whenever I felt like it. I had to inform a hospital staff member that I needed ‘a release.’ They would then get a small, rounded tray and place it underneath me. Once I was all set, they took it away. This process repeated too many times to count each day. When I first started the diuretics, I felt like I was going to be pissing out gallons at a time. As the days passed and my fluid buildup shrank, so did my frequency of bathroom breaks. The diuretics were intense and lasted for ten days. I passed more fluid in those ten days than in a normal month, and was not upset when I was weaned off.
During this preparation time, Brook was my guardian angel. She was especially nurturing and caring through all of the tests. At least five days a week, she would take a bus from New Hampshire down to South Station in Boston and walk to Tufts from there. I could not have asked for a more supportive partner in this time.
I had lost a substantial amount of fluid from the diuretics, almost thirty pounds! “It looks like the hundreds of bathroom breaks have paid off,” I joked to Brook one day. After the diuretics came pique lines. These are small lines that enter one’s body through the neck and deliver antibiotics directly to the heart. I had these lines for five days after the diuretics. These were meant to ensure that my heart was healthy enough for surgery and as strong as possible. I was scheduled to have my surgery on August 3rd. On the 2nd , I received news that the head surgeon did not have access to his normal crew of supporting doctors and nurses, and the surgery was postponed for five days. I was completely okay with this; when it came to cutting open my body, taking things out and putting new things in, I wanted the person doing all of this to be as comfortable as possible. I amused my wife and several nurses with these comments.
Heck, if the surgeon wanted me to be dressed like a clown for the surgery, I wouldn’t have asked questions if it meant he was more comfortable.
During the days leading up to the surgery, I was left to my own devices: no diuretics or pique lines. It felt good to not have to worry about taking large doses of medicine or to be undergoing intense treatment. The day after the pique lines I woke up to a surprise: I had a roommate. I welcomed him to the hospital and we immediately started sharing stories. He introduced himself and told me he was a Boston firefighter. He explained that he had suffered a heart attack when fighting a large house fire. He was older than me, but still young. I didn’t ask his age, but guessed that he was somewhere in his mid-thirties. He showed Brook and I pictures he had of his kids, two beautiful little girls. This amazing man was great at both providing conversations and excellent moral support. He talked about his job and the amazing stories that went along with it, and I talked about my racing background and how I hoped that would translate into a business someday. On the day before my surgery, he was cleared and discharged. We wished each other luck and embraced. I felt a tear building as I said goodbye.
Even though I will probably never cross paths with that man again, I will never forget him for as long as I live.
The day before surgery I was daydreaming, thinking that I wanted to do something ground-breaking after recovery. Something that most people would think was impossible to do.
I was browsing through a magazine to pass the time while Brook was making her way to the hospital from the train station. It was a sports magazine, the only one that could hold my attention out of the entire pile of magazines next to my bed. As I turned the page from an article on a football star, I came upon the centerfold spread of that issue. There was a collage of images of an athlete running, biking and swimming. ‘Oh wow, he’s a triathlete,’ I thought to myself.
I read the short column stuffed onto the side of the page and learned that this athlete was a regular Ironman participant. The article went on to explain that the Ironman races are widely considered the most grueling and demanding single-day races. This guy regularly raced a 2.4-mile swim, a 112-mile bike ride and a full marathon, 26.2 miles. These numbers blew my mind; I think my jaw actually dropped when I read this. Any one of those three events is grueling and takes so much effort. Doing all three of them back-to-back, that was intense. I found myself inspired and motivated. I decided that if I could do (almost) a short triathlon with next to no time to prepare, I could certainly work my way to an Ironman race.
I had just finished reading the article for the third time when Brook walked in. I handed her the magazine and asked her to read the article. She did, and was just as impressed as I was.
“Makes even the triathlon you competed in seem small, huh?”
“Yeah! Which is why after I’m recovered I’m going to train as much as I need to and do an Ironman race,” I threw out matter-of-factly.
Brook stared at me as if I had grown a second head. She shifted in her chair, straightened up and cleared her throat. “Jeremy, I think before you go into surgery for your heart, you should call the doctor in and have him check the condition of your brain. An Ironman race? The race finishes with a marathon. Finishes with a marathon. That’s after over a hundred miles on the bike and a massive swim. These racers must eat nails and grits for breakfast. That is insanity, you’re nuts. Your goal should be to get out of the hospital. Anything that uses a marathon for one third of the entire race is ridiculous.” I pointed out my slight success with the triathlon on short notice, but Brook stood her ground that an Ironman was a stretch.
“Just you watch. I’ll ask the doctor when he comes in, and he’ll tell you that I’ll be able to do it!’ My wife sighed and dropped the topic for the time being. When the doctor walked into the room several minutes later, I immediately called him over. “So doc, I want to do an Ironman race after I recover from surgery.” I handed him the magazine article and asked him his opinion. He closed the magazine, set it back on the table and looked at me.
“Jeremy, I think you should get better first and dream later.” That statement hurt. Brook gave me a knowing but sympathetic gaze accompanied by a faint smile. “Speaking of that, do you mind telling me what you normally do for physical activity?” I explained about my martial arts classes, my job as a fitness coach and my own personal training. After I was done and the doctor had taken in all of the information, he gave me some news that I was not all too happy to hear.
“To be completely honest with you, I think you should seriously consider shelving at least your martial arts training. After this surgery, you will be on blood thinner medication for the rest of your life. Based on what you just described, the risks of serious injury or complications you would be running by continuing martial arts seems dangerous. Even the other physical activity seems aggressive for your position.”
I set my jaw and nodded in silence. He could tell I was not pleased, and apologized. He left Brook and me alone in the room. I knew that openly defying the doctor to his face would have gotten me nowhere and only created unneeded tension. However, I also knew that voluntarily stopping martial arts was just as likely as voluntarily stopping breathing. Taking it slightly easier with the hard, heavy striking and sparring was an obvious move, but stopping was not an option. And as for the Ironman race, I had made a goal and made up my mind. I wanted to prove to my wife and the doctor that their scoffing and nay-saying was for naught.
That night Brook wished me luck, as I would be heading into surgery the following morning. She left early so that I could get plenty of rest. Just as with the endocarditis, I would be up in the wee hours of the morning and into surgery before most people are up for work. I closed my eyes that night knowing that the next day would bring about a totally different way of life for me.
On August 8th, two and a half weeks after being admitted to Tufts for heart failure, I was prepared for open-heart surgery, as was the team of miracle workers that would be making the surgery happen. The early morning preparations went off without a hitch. As I was pushed through the halls, I caught glimpses of the morning sky. It wasn’t much to look at: grey overcast clouds shrouded the horizon. The sun was trying to shine through, but the clouds refused to give way.
My heart was beating in anticipation as the large double doors to the operating room came into view. I had been preparing for this day for the past two weeks, and was determined to get through this. I looked at this as simply another challenge to overcome, another opponent to spar, another hill to climb. The lead surgeon had his team assembled and was ready to go the minute I was wheeled into the operating room. After shifting their tools around, I was given a sedative and asked to count to ten. I had only gotten to ‘two’ from my endocarditis, and I was determined to top that performance. I pushed through and barely mustered a weak ‘four’ before slipping into unconsciousness. u


 View Print Edition
View Print Edition